Muscle at Rest
Insertional activity (normal):
An electrical injury potential; it represents discharges mechanically provoked by disrupting the muscle cell membrane with a needle electrode
Confirms needle placement in muscle
After the electrical activity caused by the irritation of the needle insertion subsides, the electromyograph should detect no abnormal spontaneous activity
End Plate Noise (normal)
Endplate Potentials: caused by needle insertion into the neuromuscular junction causing leakage of acetylcholine that cause very small depolarizations in the postsynaptic muscle membrane
Low-amplitude, monophasic negative potentials firing irregularly at 20-40 Hz
Characteristic “sea shell sound”
Endplate Spikes: needle induced irritation of a terminal nerve twig and subsequent activation of a nerve action potential leading to a muscle fiber depolarization
Biphasic with initial negative (upward) deflection
Cracking, buzzing or sputtering sound on EMG
Spontaneous Activity (abnormal)
Defined as any activity at rest longer than 300ms after brief needle movement
It is among the most important information gained during the study, because:
The distribution of abnormal spontaneous activity may suggest the neuroanatomic localization of the lesion
Amount of activity suggestive of severity, while type of activity suggestive of time course
Fibrillation Potentials
Electrophysiologic marker of active denervation
Morphology: brief spike with initial positive (downward) deflection, triphasic, 1-5ms duration and low amplitude (10-100uV)
Firing pattern is very regular (0.5-10Hz) occasionally up to 30Hz
Sounds like “rain on the roof”
Typically associated with neuropathic disorders may be seen in some muscle disorders (especially inflammatory myopathies and dystrophies)
Positive Sharp Waves
Spontaneous depolarization of a muscle fiber
Same significance as fibrillation potentials
Morphology: brief initial positivity followed by a long negative phase
Amplitude is variable (10-100uV, occasionally up to 3mV)
Regular firing pattern 0.5Hz-10Hz, occasionally up to 30Hz
Usually accompanied by fibrillation potentials but may be seen alone, sometimes in early denervation
Complex Repetitive Discharge (CRD)
Result from depolarization of a single muscle fiber followed by ephaptic spread to adjacent denervated fibers (i.e., direct spread from muscle membrane to muscle membrane)
Morphology is that of individual muscle fibers that fire consecutively and are time linked together
High-frequency (20-150Hz), multi-serrated repetitive discharges with abrupt onset and termination
CRDs are identical in morphology from one discharge to another, creating a characteristic machinelike sound on EMG
Usually occur in chronic settings where denervated muscle fibers lie adjacent to one another
Fasciculation Potentials
Single, spontaneous, involuntary discharge of an individual motor unit
Fire very slowly 1-2Hz, unlike voluntary motor units which start firing at 4-5Hz with slight contraction
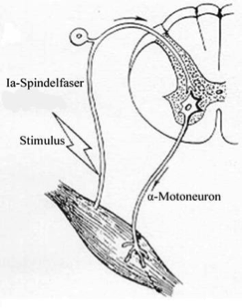
Source generator is the motor neuron or axon, prior to its terminal branches
Morphology can be simple or complex and large if they represent pathologic (re-innervated) motor unit
Sounds like “corn popping”, dull irregular pops
Seen in MND, radiculopathies, polyneuropathies, entrapment neuropathies, benign fasciculation syndrome
Analysis During Voluntary Muscle Contraction
Motor Unit Action Potentials:
Motor Unit = anterior horn cell, axon, NMJ, and muscle fibers
The extracellular needle EMG recording of a motor unit is the Motor Unit Action Potential (MUAP)
MUAP Duration
Reflects the number of muscle fibers within a motor unit
Measured from initial deflection from baseline to final return of MUAP to baseline
Typical duration is 5-15ms
Decreases with the loss of muscle fibers (myopathy)
Increases with collateral neuron sprouting (neuropathy)
Duration represented by pitch - long duration MUAP sound dull, short duration MUAP sound crisp
MUAP Amplitude
Measured from peak to peak
Most MUAP have amplitude greater than 100uV and less than 2mV and varies widely among normal individuals
Technically amplitude equates to muscle fiber density, so it will increase if a re-innervated motor unit acquires more muscle fibers or muscle fibers hypertrophy
Small changes in amplitude are not really sensitive for differentiating neurogenic from myopathic process but if significant increase in MUAP amplitude then likely represents a neurogenic loss of muscle fibers
Amplitude of MUAP correlates with volume not pitch
Number of Phases
Represents the synchrony of muscle fiber action potentials firing
MUAPs are generally triphasic
Increased phases >5 = polyphasia
Increased polyphasia beyond 10% in most muscles and 25% in deltoid is abnormal
Hear a high frequency “clicking” sound
Nonspecific measure than may be abnormal in both myopathic and neuropathic conditions
Satellite potentials: slowly conducting small MUAP that represents a new collateral sprout that trails the main MUAP; seen in early re-innervation

Neuropathic: reinnervation, the number of muscle fibers per motor unit increases resulting in long duration, high-amplitude, polyphasic MUAPs
Myopathic: loss of muscle fibers leads to short duration, small amplitude, polyphasic MUAPs
Recruitment and Firing Rate:
Recruitment: Successive activation of additional motor units to increase the force of a contraction
Firing Rate: The number of times a MUAP fires per second
Generating Force - The Rule of 5’s
The first MUAP begins firing at approximately 5Hz, when the firing rate reaches 10Hz a second MUAP begins to fire at 5 Hz; by the time the first MUAP fires at 20Hz at least 4 other MUAPs will be firing (ratio 1:5)
How to calculate from the EMG screen:
Screen width 10div x 20msec/div = 200msec
Hz = 1 cycle/sec = 1cycle/200msec x 1000msec/sec = 1000/200 = 5Hz frequency of MUAP firing if only one unit is seen per 200msec screen
If two are seen on the screen then the MUAP is firing at 10Hz, 3 units then 15 Hz, 4 units 20Hz etc.
Neuropathic Recruitment (abnormal)
Reduced recruitment: Firing of only a few MUAPs even with maximal contraction, commonly seen in neuropathic conditions
Acute Axonal Loss: decreased recruitment pattern in weak muscles due to loss of motor units; MUAP morphology remains normal
Chronic Axonal Loss: reinnervation occurs through collateral sprouting of adjacent surviving motor units; as the number of muscle fibers per motor unit increases the MUAPs become prolonged in duration, high amplitude and polyphasic; this in conjunction with reduced recruitment is the hallmark of chronic neuropathic disease
Pure demyelinating lesions with conduction block can show reduced recruitment with normal MUAPs
Myopathic Recruitment (abnormal)
Acute: number of functioning muscle fibers in a motor unit decreases
MUAPs shorter duration and smaller amplitude
Less synchronous firing and dysfunction of remaining muscle fibers leads to polyphasia
Early recruitment: each motor unit contains fewer fibers and cannot generate as much force as a normal motor unit
To compensate more MUAPs will fire than are normally needed for a certain level of force
Chronic:
In many chronic myopathies two populations of MUAPs are often seen: both long duration, high amplitude, polyphasic MUAPs due to denervation and subsequent reinnervation and short duration, small amplitude, polyphasic MUAPs
The key to differentiating chronic myopathic from chronic neuropathic MUAPs is the assessment of recruitment pattern: recruitment appears normal or early
End Stage:
- The actual number of motor units may effectively decrease if every fiber of the motor unit dies or becomes dysfunctional; this can lead to an unusual pattern of reduced recruitment of myopathic appearing motor units +/- long duration, high amplitude, polyphasic MUAPs
Activation
Ability to increase firing rate
This is a central process
Poor activation may be seen in disease of the central nervous system or as a manifestation of pain, poor cooperation, or functional disorders
Interference Pattern
During maximal contraction, multiple MUAPs normally overlap and create an interference pattern in which no single motor unit can be distinguished
The interference pattern depends on both activation and recruitment
An incomplete interference pattern may be due to either poor activation or poor recruitment
-
Both decreased activation and decreased recruitment can occur in the same patient
Ex. ALS (UMN and LMN dysfunction)
Ex. Painful radiculopathy (Reduced recruitment and decreased activation due to pain)
Suggested Readings
Electromyography and Neuromuscular Disorders by David C. Preston and Barbara E. Shapiro
Electromyography in Clinical Practice: A Case Study Approach by Bashar Katirji