PATIENT ASSESSMENT
BP/Glucose:
Times: Last known normal, Symptom onset, Stroke Code, Evaluation by Neuro, CTH Read
Anticoagulation: warfarin, heparin, DOAC
Medical History: ICH, AVM, Aneurysm, Recent surgery or trauma, Recent MI, Recent bleeding, recent LP
CT Scan (+/- Blood)__________________________________________________
IV tPA INDICATIONS
The following 5 boxes must be checked to give IV tPA:
Diagnosis of acute ischemic stroke
Definite time of onset
Diagnosis of ischemic stroke causing measurable neurologic deficit
Non-contrast CT head showing no hemorrhage or well-established new infarct
Onset of acute stroke symptoms within 3 hours (Between 3-4.5 hours from symptom onset, selected patients may be eligible for tPA).
IV tPA CONTRAINDICATIONS
IV or IA tPA given for these symptoms at an outside hospital
Non-contrast CT head showing hemorrhage or well-established new infarct
Systolic BP > 185 and Diastolic BP > 110 despite treatment
History of intracranial hemorrhage, or known intra-axial brain tumor at the discretion of the treating neurologist
Intracranial or spinal surgery, or serious head trauma within the last 3 months at the discretion of the treating neurologist
Gastrointestinal Hemorrhage within the last 21 days at the discretion of the treating neurologist
Symptoms consistent with infective endocarditis OR aortic arch dissection
Suspicion of subarachnoid hemorrhage by imaging or clinical presentation
Platelets < 100,000/mm3, PTT not within normal range after IV heparin use, INR > or = 1.7, or other known bleeding diathesis
Note: DOACs
In patient taking dabigatran whose last dose was at least 12 hours ago or who PTT is within normal limits, IV alteplase may be considered
In Patients taking oral factor Xa inhibitors whose last does was at least 48 hours ago or whose direct factor Xa assay is within normal limits, IV tPA may be considered
tPA RISKS/BENEFITS
These should be discussed with the patient and family, although tPA administration does not require consent as it is standard of care for eligible patients.
tPA for acute stroke decreases disability at 3 months and does not increase risk of death (NINDS)
The NINDS study suggested that bleeding into the brain occurred in about 1 out of 18 patients receiving tPA (specifically, 5.8%). When this occurred, there was a 45 percent fatality rate.
IV tPA PATIENT MANAGEMENT
Prior to Infusion:
-
Call the ED pharmacist or the pharmacy tPA hotline at x7-8789 for all cases requiring tPA preparation, regardless of patient location or time of day.
ask pharmacist to start mixing as soon as you suspect that you will want to give tPA
mixed but unused bottles of tPA can be replaced free of charge
Obtain the patient’s weight. If unavailable, use 2 person estimate.
Make sure that the patient has 2 IVs (at least one of which is 20-gauge).
Procedures pre-tPA - placement of central venous access, arterial punctures
Do not delay tPA for placement of the following - NG tube, foley catheter, or additional IV line. These can be performed after tPA administration.
Do not delay tPA for CTA. Can mix tPA while CTA is running.
-
If SBP>185 or DBP >110
Labetalol 10-20 mg IV over 1-2 min; may repeat x 1 OR
Clevidipine infusion 0.5mg/mL - Initial dose 1-2 mg/hr IV -> Double the dose every 90 seconds until desired BP, OR
Nicardipine 5 mg/hr IV infusion -> titrate to desired effect by increasing 2.5 mg/hr every 5 minutes to maximum of 15 mg/hr -> when at goal BP, reduce to 3 mg/hr
If BP is not reduced and maintained at desired levels (systolic ≤ 185 + diastolic ≤ 110), do NOT give IV tPA
IV tPA Administration:
perform tPA time out with RN and pharmacist
-
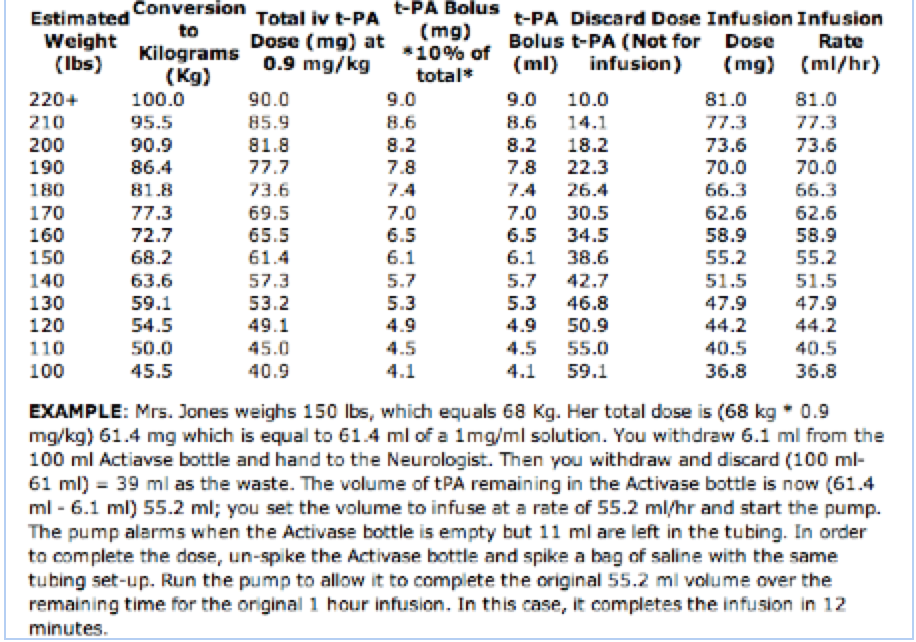
Give 0.9 mg/kg (max 90 mg) tPA (alteplase, Activase) - document time that bolus is given
give 10% of the total dose administered as an initial IV bolus over 1 min (1 lb = 0.45kg)
infuse remaining 90% over 60 min
tPA should not be stopped for CTA or other medications
Post-tPA Management:
Required Orders and Documentation:
Place post-tPA orders (post tPA ischemic stroke order set)
Conduct and document post-tPA huddle (smartphrase STROKEHUDDLE)
Conduct and document hourly check-ins (smartphrase STROKECHECKIN)
3oz swallow screen
Beginning with administration of the tPA bolus, vital signs and neurologic assessments are performed and documented by the nurse on the tPA Flowsheet:
Every 15 minutes x 2 hours (includes the hour of IV tPA administration)
Then every 30 minutes x 6 hours
Then every 60 minutes x 18 hours
Perform a post-tPA huddle at bedside that includes ED resident, ED RN, ED attending, to communicate:
Blood pressure targets
Cardinal sign (one aspect of NIHSS other than LOC or motor function)
Baseline NIHSS
Contact number to reach Neurology resident directly
Additional Considerations:
During and after the tPA infusion, increase the frequency of blood pressure measurements if SBP >180 or if DBP >105 mm Hg (see guide below)
While patient remains in the ED waiting for a stroke unit or NSICU bed, perform hourly checks with the patient to ensure exam grossly stable and BP within range
If the patient develops severe headache, acute hypertension, nausea, or vomiting, or new focal neurologic deficits, stop the infusion (if IV tPA is being administered) and obtain emergent CT scan. If there is nothing to suggest that IV tPA is causing these symptoms, infusion may be resumed.
Patients who receive IV tPA and are eligible for intra-arterial intervention may go on to receive acute procedural and post-procedural anti-coagulants or anti-platelet medications based on the procedure performed and judgment of the treating physicians.
MANAGEMENT OF tPA COMPLICATIONS
Arterial Hypertension:
Labetalol 10-20 mg IV over 1-2 min; May repeat or double every 10 to 20 minutes to a maximum dose 300 mg or give the initial labetalol bolus and then start a labetalol drip at 2 to 8 mg/min OR
Clevidipine infusion 0.5mg/mL - Initial dose 1-2 mg/hr IV -> Double the dose every 90 seconds until desired BP, OR
Nicardipine 5 mg/hr IV infusion -> titrate to desired effect by increasing 2.5 mg/hr every 5 minutes to maximum of 15 mg/hr -> when at goal BP, reduce to 3 mg/hr
If BP still not controlled after the above options have been exhausted, consider sodium nitroprusside (discuss with supervising fellow or attending)
Management of angioedema:
Discontinuation of the tPA infusion
Administer diphenhydramine 50 mg IV and Famotidine 20 mg IV
If tongue continues to enlarge, give methylprednisolone 80-100 mg IV
-
If any further tongue enlargement:
Give epinephrine 0.1% 0.3 mL SC or 0.5 mL via nebulizer
Call ENT, anesthesiology or other appropriate in-house service STAT for possible emergent cricotomy, tracheostomy or fiberoptic nasotracheal intubation if oral intubation unsuccessful (secondary to impending airway obstruction)
Management of Arterial Hypotension:
Correct potential causes including volume replacement with normal saline for hypovolemia
Consider vasopressors as clinically indicated
Treatment of Intracranial Hemorrhage after IV tPA:
Stop tPA infusion; check CBC, PT, PTT, platelets, fibrinogen, DDimer
Administer cryoprecipitate (0.15 units/kg) ~ 10 units
If still bleeding at 1hr and fibrinogen still <100 mg/dL repeat cryoprecipitate (0.15 units/kg).
Consider aminocaproic acid 4-5 g IV or, if not available, tranexamic acid 1g IV
If the patient has clinical deterioration or enlargement of ICH on repeat Head CT (after anticoagulant or antiplatelet reversal), additional correction / reversal agent should be given.
Acute Management of Patients NOT Eligible for IV tPA or Intra-Arterial Interventions:
-
Permissive BP to SBP 220 OR MAP 100, unless signs of hypertensive emergency w/end-organ involvement, e.g aortic dissection, acute myocardial infarction, pulmonary edema, or hypertensive encephalopathy. If indicated:
Labetalol 10-20 mg IV over 1-2 minutes; May repeat or double every 10 min (max dose 300 mg) OR
Nicardipine 5 mg/hr IV infusion as initial dose; titrate by increasing 2.5 mg/hr every 5 min to max of 15 mg/hr
Aim for a 10% to 15% reduction in blood pressure
Administer an antithrombotic agent (consider aspirin per rectum if NPO or by mouth if dysphagia screening performed by neurology/stroke service and patient safe to swallow medications)
Repeat vital signs every 2 hours or as determined by the stroke team while patient remains in emergency department with presumptive diagnosis of acute stroke.